Repairing traumatic injury to a bone is do-able, but current procedures require multiple surgeries and long term recovery. Kettering University’s Dr. Montserrat Rabago-Smith and her team of co-researchers are exploring the use of a magnesium orthotic alloy in severe trauma injuries where the distance between two halves of a bone can’t be overcome by the human body’s ability to regenerate and heal.
They are trying to develop a magnesium alloy material that is biodegradable and requires only one surgical procedure to assist the bone in healing over the “magic” distance. “A magic distance is two times the width of the bone that is damaged,” she explained.
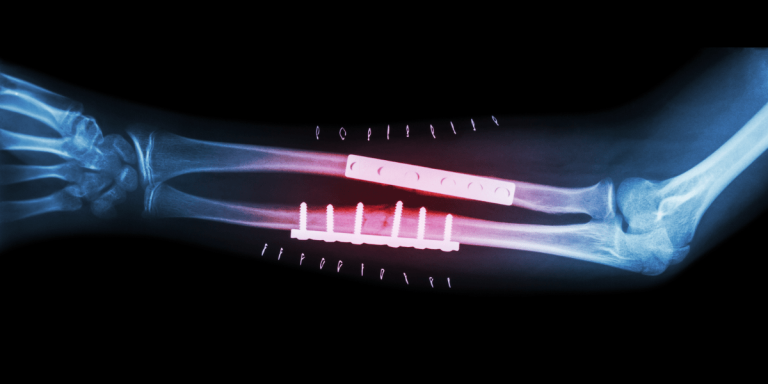
“Currently surgeons put a titanium or stainless steel rod in the gap to save what is usually a severely damaged limb,” said Rabago-Smith, assistant professor of Chemistry/Biochemistry at Kettering. “This requires two major surgical procedures, one to implant the rod and a later surgery to remove the screws holding it in place,” she said.
If this rod is left in the body for a long period of time, bone can build up around the ends of the rod, making it difficult to remove the screw and creating other problems such as an inflammatory reaction due to the titanium alloy shedding small pieces or leaching materials into the surrounding tissue.
The goal of the research is to help to bridge the “magic gap.” “Human cells can only travel so far in the healing process,” Rabago-Smith explained, “so what seems like a small distance is actually quite far on a cellular level.” Their research is focused on developing biomaterials that can be absorbed by the body and that will dissolve as the bone grows and repairs.
Magnesium alloy was chosen as an orthopedic biomaterial for its bioresorbable properties. Its mechanical properties are similar to natural bone, making it appropriate for load-bearing orthopedic fracture repair applications. Non-biodegradable implants are unable to adapt to growth and changes of the human body, and the strength and density of titanium alloys greatly exceed that of bone, causing stress shielding, according to the research by Rabago-Smith and her colleagues.
This stress shielding may compromise the integrity of new bone growth and the quality of existing bone. The strength and density of Magnesium and Mg alloys match those of bone while also being stronger than bone, and so are less likely to cause stress shielding.
“Our alloy, Mg AZ31, is shaped like a tube and coated with a substance that helps to control the degradation of magnesium alloy,” she said. The tube shape was designed in an effort to reduce the amount of alloy used for implantation in a shape that mimics cortical bone shape. Details of their work will be published in the Journal of Biomedical Materials Research Part B, according to Rabago-Smith.
This hollow cylinder acts as a scaffold for bone re-growth. The scaffold was then coated with different amounts of the coating developed by Rabago-Smith and her colleagues and immersed in simulated body fluid (SBF) and enhanced biocompatibility for mesenchymal stem cells (MSC). The coated scaffold showed a slowed corrosion compared to non-coated scaffolding.
Rabago-Smith developed the coating that slows the degradation, and then tested its healing properties with fellow researchers, Dr. Xingguo Cheng, Senior Researcher at Southwest Research Institute, Biomaterial and Biochemistry Section, Department of Microencapsulation and Nanomaterials, Dr. Patrick Atkinson, professor of Mechanical Engineering at Kettering, and Desiree White and Tyler Piersma, both 2011 graduates of Kettering. Other collaborators from the Southwest Research Institute included Dr. Gloria Gutierrez, Dr.Gianny Rossini, Dr. Stephen Wellinghoff and Sapna Desai.
“Magnesium is very reactive by itself, especially in the presence of water where the reaction occurring is oxidization, like rust,” said Rabago-Smith. “Inside the body it will corrode rapidly due to the water and acids present in human tissue.
“The coating protects a little, but not completely, so degradation does occur,” she said, but went on to explain that the degradation is gradual, and slow “like a long term fish pellet,” giving the body time to generate new bone. “Our scaffold facilitated new bone growth across the magic distance,” she said.
The gradual release of Mg2+ is not expected to lead to toxic reactions because Mg concentration in the body is high and tightly controlled.
Rabago-Smith and her colleagues are still in the process of studying the coating and improving the process. Their goal is to improve bone growth and develop a biodegradable material. However, it is still not appropriate for use in humans and significant hurdles remain regarding the design of practical implants and methods to control the alloy’s degradation in the human body and biocompatibility.
To date, their findings have been presented by Kettering graduates White, Piersma and David LeCronier ’06, at the 2010 and 2011 Research Exhibition of Excellence hosted by Michigan State University’s Flint Area Medical Education program and Rabago-Smith presented them at the Michigan Orthopedic Society’s Annual Scientific Conference in June 2010 and 2011 on Mackinac Island.
Contact: Dawn Hibbard
810.762.9865
dhibbard@kettering.edu